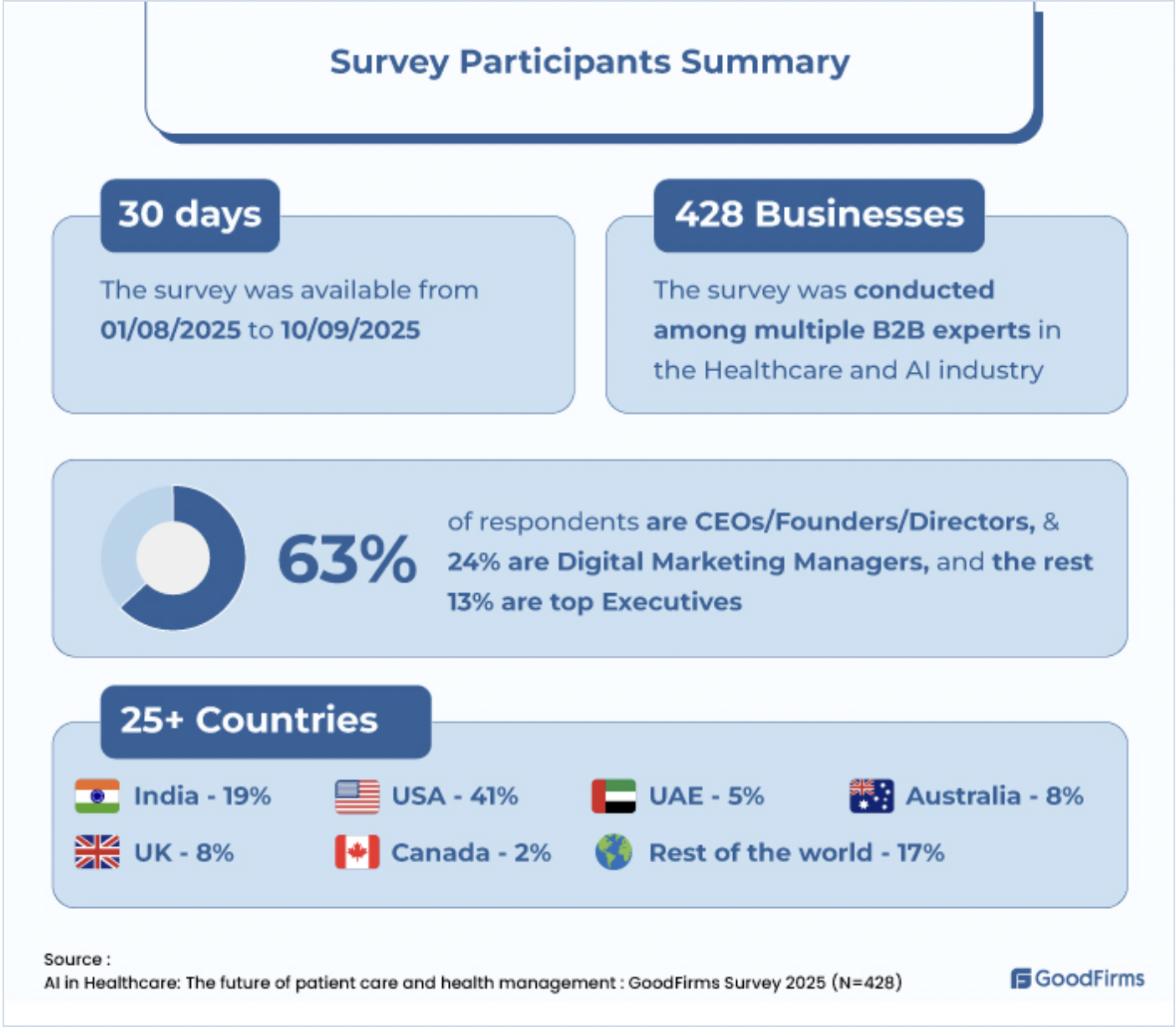
The landscape of healthcare is on the cusp of a revolution, not one led solely by a new pharmaceutical breakthrough, but by the silent, pervasive power of artificial intelligence. As detailed in research by GoodFirms, AI is rapidly transitioning from a futuristic concept to a practical toolset, fundamentally reshaping patient care management from a reactive model to a proactive, personalized, and highly efficient system. By augmenting human expertise with data-driven intelligence, AI is poised to enhance every stage of the patient journey, from diagnosis and treatment to long-term wellness, heralding a new era of precision medicine and democratized care.

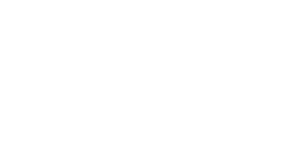
The most immediate and profound impact of AI lies in the realm of diagnostics and medical imaging. Traditional methods of analyzing MRIs, CT scans, and X-rays are time-consuming and subject to human fatigue and error. AI algorithms, particularly those based on deep learning, are now being trained on vast datasets of medical images, enabling them to detect anomalies with a speed and accuracy that often surpasses human capabilities. The GoodFirms research highlights how AI can identify early signs of diseases like cancer, cardiovascular conditions, and neurological disorders long before they become apparent to the human eye. This capability for early and accurate detection is not merely an incremental improvement; it is a paradigm shift that can significantly increase survival rates by enabling interventions at the most treatable stages of disease. This transforms patient care management by providing a more reliable and swift foundation upon which all subsequent treatment decisions are built.
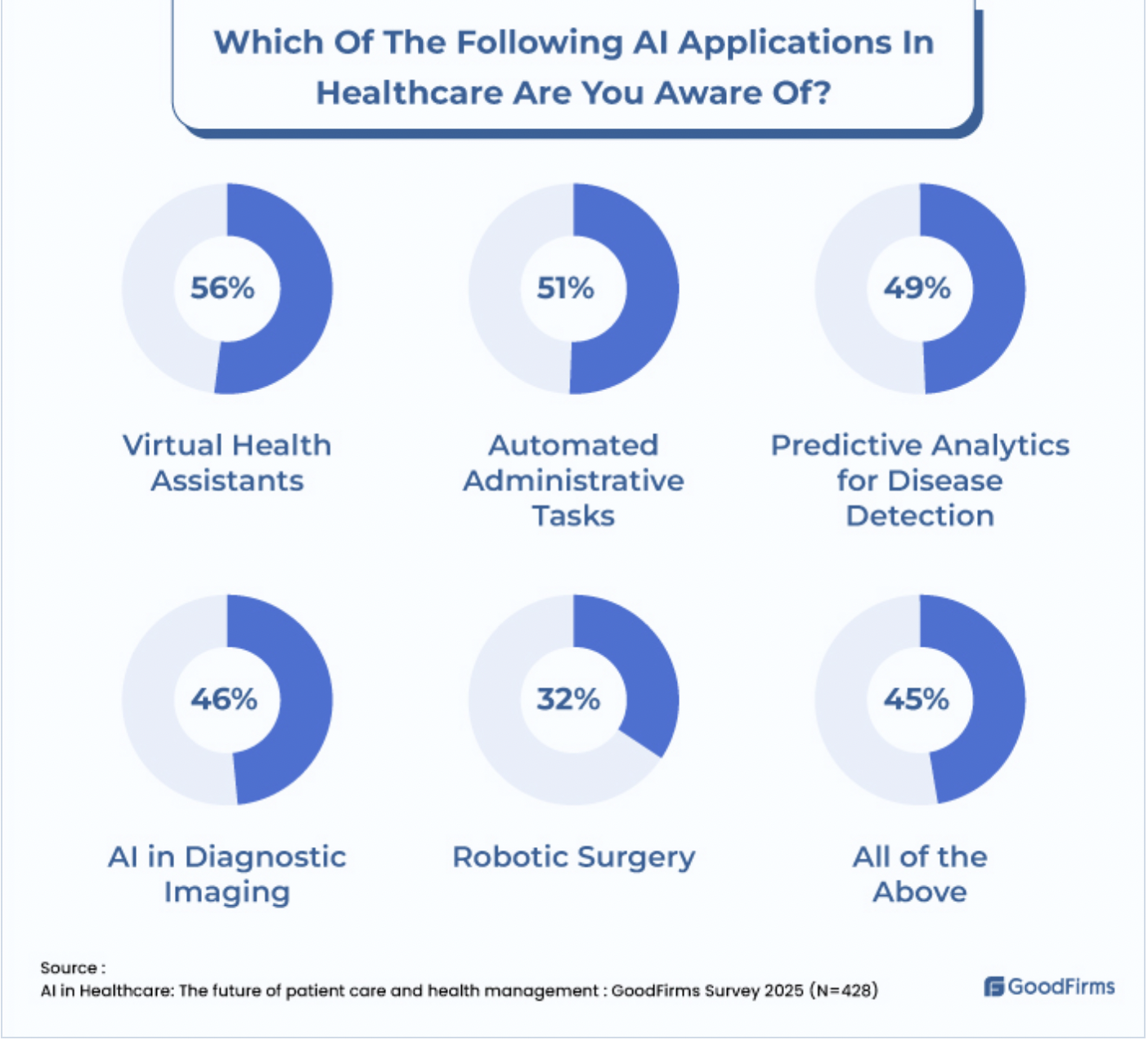
Beyond diagnostics, AI is the engine powering the shift towards personalized and predictive medicine. The “one-size-fits-all” approach to treatment is becoming obsolete. AI systems can integrate and analyze diverse data points—from a patient’s genetic makeup and electronic health records (EHR) to real-time data from wearable devices and lifestyle factors. This holistic analysis allows for the creation of highly tailored treatment plans. For instance, in oncology, AI can help determine the most effective chemotherapy regimen based on the specific genetic mutations of a patient’s tumor. Furthermore, as noted in the research, AI’s predictive analytics can forecast individual patient risks, flagging those susceptible to conditions like diabetes or sepsis. This moves care management from a reactive stance—treating illness after it manifests—to a proactive one, where healthcare providers can engage in preventative strategies tailored to each patient’s unique risk profile.
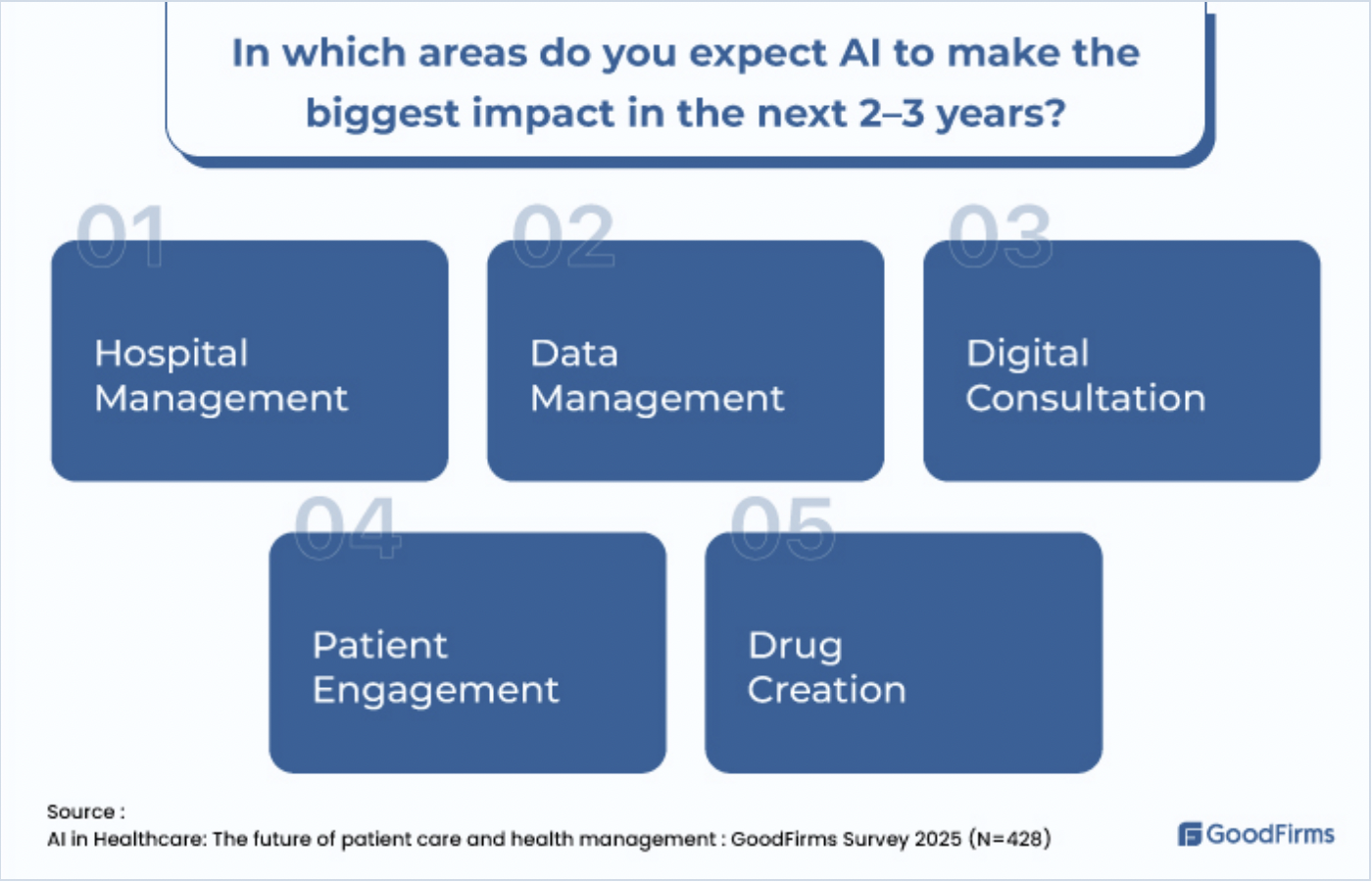
The administrative and operational burdens that have long plagued healthcare systems are also being alleviated by AI, leading to improved patient care through enhanced efficiency. A significant portion of healthcare costs and physician burnout is attributed to administrative tasks. AI-powered solutions are automating these processes, from managing electronic health records and processing insurance claims to streamlining hospital workflow and inventory management. Natural Language Processing (NLP) algorithms can transcribe and organize clinical notes, freeing up precious time for doctors to engage directly with patients. This operational efficiency directly translates to better patient care management: reduced wait times, lower healthcare costs, and, most importantly, a healthcare workforce that can focus its energy on human interaction and complex clinical decision-making rather than bureaucratic paperwork.
The integration of AI into healthcare is not without its challenges, a reality the GoodFirms research also acknowledges. The “black box” problem, where some AI decisions are not easily interpretable by humans, raises concerns about accountability and trust. Furthermore, the quality of AI is entirely dependent on the quality and breadth of the data it is trained on; biased data can lead to biased algorithms, potentially exacerbating health disparities. Issues of data privacy, security, and stringent regulatory compliance also present significant hurdles that must be navigated with care.
The research makes it clear that artificial intelligence is not a replacement for human clinicians but an indispensable ally. Its ability to enhance diagnostic precision, enable truly personalized treatment, and unburden the healthcare system of administrative inefficiencies positions it as the cornerstone of future patient care management. While challenges regarding transparency, bias, and privacy must be addressed through robust ethical frameworks and continuous oversight, the potential benefits are too profound to ignore. The future of healthcare will be a synergy of human compassion and clinical experience with the formidable analytical power of AI, working in tandem to create a system that is not only smarter and more efficient, but also more humane and proactive in safeguarding human health.